Even before the state was hit with COVID-19, the Medicaid burden had become unsustainable
Historically, Medicaid was funded almost exclusively by the federal government. Now, with the Medicaid expansion and the extension of benefits to illegal aliens, Medicaid is on the verge of becoming unsustainable both in terms of costs and the demands that it puts on resources and personnel, and these costs are being increasingly borne by the state. Medicaid programs deliver health care services to over one million people in Oregon -- about a quarter of the population -- primarily through the Oregon Health Plan, which supports comprehensive health care coverage for low-income adults and
children eligible for Medicaid, children eligible under the federal Children’s Health Insurance Program (CHIP), and
children who would be eligible for Medicaid or CHIP except for their immigration status.
Oregon's Medicaid programs have experienced significant changes in the last several years. In the 2011-13
biennium, Oregon transformed the way it provides and pays for medical assistance through a new Medicaid
health care delivery system managed by coordinated care organizations (CCOs). A CCO is a network of all types of
health care providers who agree to work together in local communities to serve OHP members. CCOs focus on
prevention; chronic disease management; early intervention; integration of physical, behavioral, and oral health;
and the reduction of waste and inefficiency in the health system.
The jury is still out on the effectiveness of CCOs to meet this mission.
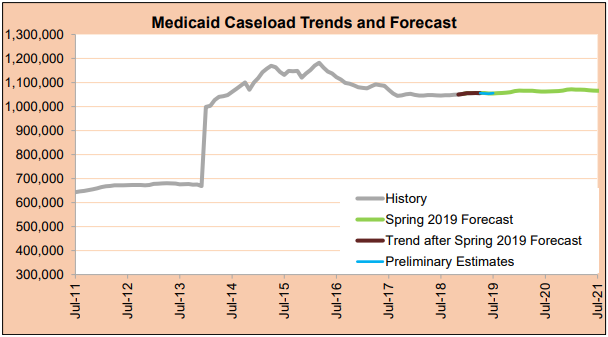
The chart at the right shows the considerable spike in caseload when Medicaid was expanded. It should be noted that the estimates that the chart was based on were made before the recent COVID-19 outbreak.
--Staff Reports, with Legislative Fiscal Office| Post Date: 2020-04-26 21:20:21 | Last Update: 2020-04-26 21:20:39 |